You wake up after a restless night and feel a scratchy throat. You wonder whether stress made you vulnerable again. Your calendar looks packed and unforgiving this week. Could your hormones be nudging immunity off course today? That question opens a useful doorway for everyday health. Let’s walk through it together with calm, clear steps.
How do hormones and immunity talk to each other?
Hormones are chemical messengers that set body priorities. Immune cells listen to these signals closely. They adjust speed, power, and duration of responses. The conversation runs every hour of the day. It changes with light, meals, sleep, and stress. Small routine choices therefore shape immune tone meaningfully.
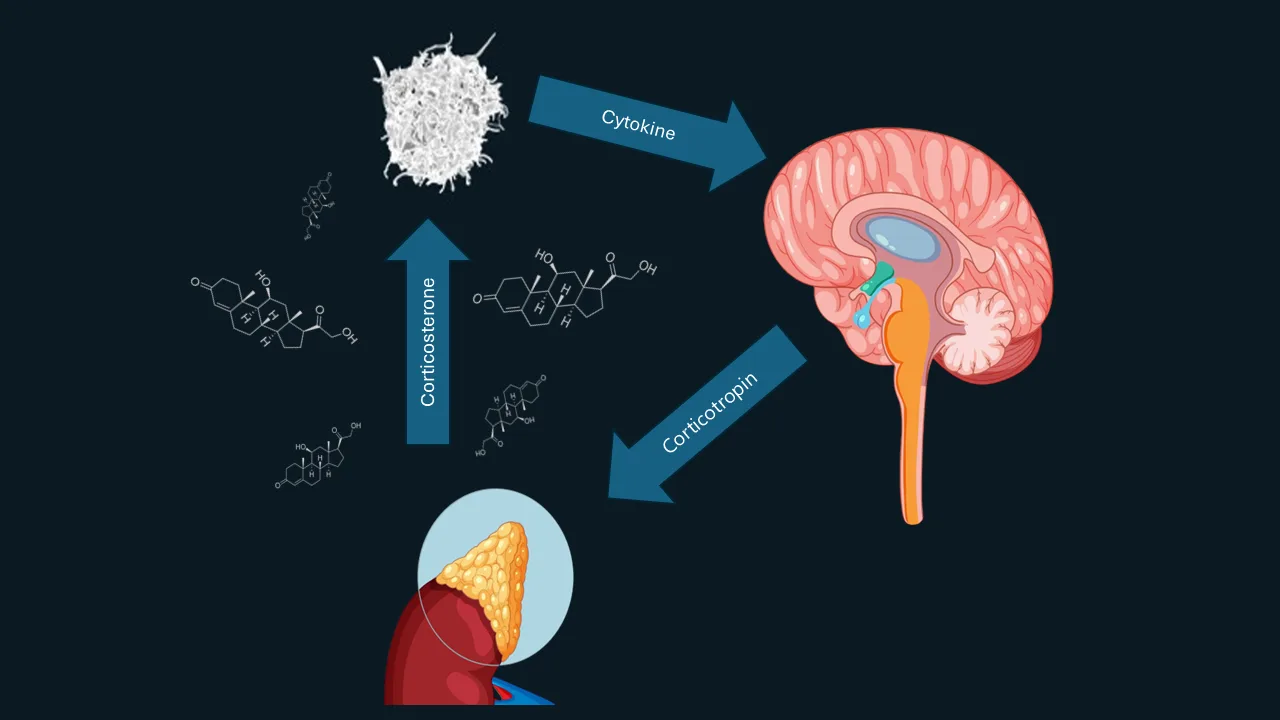
What is the HPA axis and why care?
The HPA axis links brain and adrenal glands. It helps the body manage pressure and recovery. The star hormone here is cortisol. Cortisol keeps inflammation from spiraling out of control. Too little control allows damaging flare ups. Too much control can blunt protective defenses.
How does cortisol affect everyday responses?
Cortisol follows a daily rhythm naturally. Levels peak in the early morning hours. They fall gradually across afternoon and evening. Balanced peaks help you wake with energy. Balanced declines help you fall asleep later. Disrupted rhythms can disturb immune timing and comfort.
Do adrenaline and noradrenaline change immunity?
Yes, they shape rapid responses during stress. These hormones prepare muscles and focus attention. They also signal immune cells to relocate. Some cells patrol blood, others guard tissues. Short bursts support quick, coordinated protection. Long floods can exhaust systems and slow repair.
Why does circadian rhythm matter for defenses?
Your internal clock coordinates cellular schedules. Immune cells follow that clock carefully. Night signals promote repair and tidy up. Day signals favor surveillance and quick action. Light exposure sets this master clock daily. Regular light and darkness protect immune precision.
Where does melatonin fit in this picture?
Melatonin rises in the evening darkness. It helps time sleep and nighttime repair. Immune tissues carry melatonin receptors widely. Night signals reduce noisy daytime inflammation. Late screens can suppress melatonin release noticeably. Evening dimness supports calmer overnight immune work.
How do thyroid hormones influence immunity?
Thyroid hormones set metabolic pace for tissues. Immune cells adjust to that pace directly. Low thyroid function can slow cellular responses. High thyroid function can overstimulate certain pathways. Both patterns may affect infection comfort and fatigue. Balanced thyroid care supports steadier immune rhythms.
What about insulin and metabolic hormones?
Insulin helps cells use glucose effectively. Chronically high insulin can favor inflammatory signals. Leptin and adiponectin also modulate immune tone. Central fat releases additional signaling molecules daily. These signals shape infection recovery and energy levels. Gentle nutrition and movement stabilize these patterns.
Do sex hormones change immune patterns notably?
Yes, estrogen, progesterone, and testosterone influence many pathways. Estrogen often enhances certain antibody responses. Progesterone can promote calming signals during pregnancy. Testosterone may reduce some inflammatory peaks. Differences help explain varied responses across life stages. Individual patterns still matter beyond broad trends.
How does the menstrual cycle affect immunity?
Hormone levels shift across the cycle naturally. Some people notice colds near specific phases. Others notice skin changes or mouth ulcers. Sleep and stress can amplify such patterns. Tracking symptoms reveals personal timing clues. Awareness allows smarter planning around vulnerable windows.
What immune shifts happen during pregnancy?
Pregnancy promotes tolerance toward the developing baby. Immune priorities adjust rather than shut down. Some infections become more uncomfortable during pregnancy. Vaccines may gain extra importance for families. Clinicians tailor schedules to protect parent and child. Communication keeps plans safe and reassuring.
What changes after menopause or andropause?
Estrogen and testosterone level patterns evolve with age. These shifts can influence inflammation and repair. Sleep also changes and affects rhythms further. Muscles lose mass without regular training. Joint comfort may vary across the year. Gentle routines protect function through these transitions.
Why are autoimmune conditions more common in women?
Sex hormones influence immune education and tolerance. Genetics and X chromosome factors also contribute. Microbiome differences may add further layers. Life stages reveal these differences more clearly. Personalized plans respect these real variations. Respect reduces judgment and supports effective care.
Can hormones affect vaccine responses and timing?
Hormonal status can shape antibody levels modestly. Sleep before vaccination supports better responses. Stress management also helps the body learn effectively. Hydration and nutrition keep side effects tolerable. Clinicians consider timing during pregnancy carefully. Coordination turns simple visits into durable protection.
What about infections during high stress periods?
High stress can unsettle hormonal rhythms quickly. Cortisol patterns may lose their morning peak. Sleep shortens and melatonin release shrinks. Appetite changes skew towards quick comfort foods. These shifts can invite minor infections more often. Restoring anchors brings defenses back on track.
How does the microbiome join this conversation?
Gut microbes react to hormones you release. They also produce signals that reach immune cells. Fiber and diverse foods nurture resilient communities. Extreme diets can reduce that diversity quickly. Gentle, varied meals stabilize this two way conversation. Stable conversations keep inflammation calmer overall.
Where do sleep and light upgrades start?
Choose a regular bedtime and wake time. Step into bright morning light soon after waking. Dim your environment during the last hour. Keep the bedroom cool and quiet nightly. Reserve the bed for sleep and intimacy. These basics improve hormonal timing reliably.
How should meals support hormone friendly immunity?
Aim for balanced plates with color and fiber. Include legumes, vegetables, fruits, and whole grains. Add lean proteins or fish regularly. Use olive oil or similar unsaturated fats. Keep sugary drinks for rare moments only. Eat earlier in the evening when possible.
Does exercise help immune harmony directly?
Regular activity improves insulin sensitivity meaningfully. It trains stress systems to recover faster. Moderate intensity supports antibody responses over time. Hard sessions need rest and sleep to benefit. Short walking breaks help on busy days also. Consistency matters more than occasional extremes.
Are environmental disruptors worth attention now?
Certain chemicals can mimic hormones in tissues. Plastics and pesticides appear in many products. Ventilation reduces indoor exposures noticeably. Choose simple cleaning products when possible. Avoid overheating plastic containers in microwaves. Small habits reduce avoidable background noise.
How do puberty and adolescence shape immune learning?
Puberty introduces new hormonal patterns quickly. Skin and airway responses may shift dramatically. Sleep needs rise while schedules often fight them. Nutrition quality fluctuates with social rhythms. Vaccination schedules consider these transitions carefully. Guidance helps families protect comfort and confidence.
What about contraceptives and immune comfort?
Hormonal contraceptives adjust estrogen and progesterone exposure. Some people notice fewer cyclical symptoms. Others notice different skin or mood patterns. Discuss changes with your clinician openly. Update your medication list at each visit. Personal comfort guides refinements over time.
How does chronic illness interact with hormones?
Diabetes, thyroid conditions, and kidney issues shift signals. Immune priorities adapt to these backgrounds daily. Medicine timing can affect rhythm quality noticeably. Pillboxes and reminders keep schedules steady. Regular labs prevent quiet drifts from targets. Steady control reduces infection surprises.
According to our editor’s research, what habits help most?
According to our editor’s research, three anchors stand out repeatedly. People who walk outdoors most mornings report steadier energy. Households that dim lights nightly fall asleep faster. Families that plan earlier dinners notice calmer digestion. These anchors support hormone timing and immunity.
As a result of our editor’s reviews, which tools work smoothly?
As a result of our editor’s reviews, light systems beat complex apps. A simple alarm protects bedtime consistently. A kitchen timer ends late screens without arguments. A weekly grocery list preserves balanced meals. A small notebook tracks cycle related symptoms. These tools keep change realistic and kind.
Where do official recommendations fit locally?
Health ministries publish vaccination and sleep guidance yearly. Endocrine and immunology societies update practice summaries. Occupational bodies advise on shift worker strategies. National nutrition programs share practical plate models. These groups present careful, consensus based advice. Their messages match everyday clinic experience closely.
When should you see a clinician about hormones?
Seek care for persistent fatigue despite solid sleep. Report night sweats or unexplained weight changes. Discuss mood shifts that last several weeks. Ask about thyroid and metabolic checks when concerned. Consider reproductive hormone discussions when cycles change. Bring notes about timing, sleep, and meals.
How can you build a practical weekly plan?
Pick one change for mornings and one for evenings. Morning sunlight can be the first step. Evening dimness can be the second step. Add a short walk after two weeks. Pair protein and fiber at lunch regularly. Keep a bedtime within a one hour window.
Why does kindness matter during behavior change?
Rigid plans break during real life pressure. Gentle plans bend and continue afterward. Celebrate partial wins during tough weeks. Ask for support before motivation fades. Return to anchors after travel or illness. Kindness keeps progress alive across seasons.
What signs suggest progress this month?
You fall asleep faster most nights. Morning energy rises more consistently. Afternoon cravings feel quieter and shorter. Workouts feel easier at similar effort. Minor colds resolve more quickly overall. Mood steadiness holds during busier days.
Where do culture and family habits shape success?
Shared meals set timing and ingredients daily. Family sleep schedules affect everyone’s rhythms. Community traditions may influence evening light. Work hours often shape movement opportunities. Align changes with these realities kindly. Tailoring improves comfort and adherence.
How should you discuss these ideas with kids?
Use simple words about sleep and light. Explain why breakfast matters for school focus. Keep screens outside bedrooms at night. Encourage movement as play whenever possible. Praise effort rather than perfection openly. Small routines teach lifelong resilience gently.
What about travel and jet lag effects?
Jet lag scrambles hormonal timing temporarily. Seek morning light at your destination. Eat local daytime meals promptly. Nap briefly but avoid long daytime sleep. Hydrate and move during flights regularly. Give your body two or three days to reset.
Can breathing practices support hormonal calm?
Slow breathing lowers sympathetic activity gently. Inhale through the nose for four counts. Exhale for six counts comfortably. Repeat for several minutes each evening. Pair with dim lights and quiet music. Simple routines can tame daily stress.